胆固醇偏高会影响入职
My previous article discussed gender and ethnicity differences in prevalence of diabetes and diabetes-related mortality rates for states encompassing the diabetes belt. This data came from the CDC’s Chronic Disease Indicators (CDI): Diabetes dataset, which provides a compilation of diabetes-related information for all states and territories from 2010 to 2018.
我的前一篇文章讨论了糖尿病患病率的性别和种族差异以及与糖尿病相关的各州的糖尿病相关死亡率。 该数据来自CDC的慢性疾病指标(CDI):糖尿病数据集 ,该数据集提供了2010年至2018年所有州和地区的糖尿病相关信息。
In this article, I want to use the data from the CDI Diabetes dataset to explore the relationship between diabetes and its comorbidities: high blood pressure and high cholesterol. Just like diabetes, these two comorbidities are known risk factors for heart disease. I would like to see if one comorbidity is more prevalent than the other, for adults with diagnosed diabetes in the diabetes belt. I would also like to see if there is a sex bias for prevalence of high blood pressure and prevalence high cholesterol among adults with diagnosed diabetes in the diabetes belt.
在本文中,我想使用CDI糖尿病数据集中的数据来探索糖尿病与其合并症之间的关系:高血压和高胆固醇。 就像糖尿病一样,这两种合并症是已知的心脏病危险因素。 我想看看对于患有糖尿病的成年人来说,一种合并症是否比另一种更为普遍。 我还想看看在糖尿病带被诊断为糖尿病的成年人中,高血压的患病率和高胆固醇的患病率是否存在性别偏见。
This exploratory data analysis was done in Jupyter Notebook/Python. The code used to produce these visualizations and statistical tests used in this article has been posted to GitHub here.
探索性数据分析是在Jupyter Notebook / Python中完成的。 用于生产本文中使用这些可视化和统计检验的代码已经被发布到GitHub上这里 。
The diabetes belt, as described by Barker et al. in 2011, includes “Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, North Carolina, Ohio, Pennsylvania, South Carolina, Tennessee, Texas, Virginia, and West Virginia, … Mississippi.” In my previous article, I focused on this subset of states, because these states are much more affected by diabetes than the rest of the country and allow for a more focused analysis. In this article, I am going to continue analyzing this data and drawing conclusions for states that constitute the diabetes belt only.
如Barker等人所述。 2011年,包括“阿拉巴马州,阿肯色州,佛罗里达州,乔治亚州,肯塔基州,路易斯安那州,北卡罗来纳州,俄亥俄州,宾夕法尼亚州,南卡罗来纳州,田纳西州,德克萨斯州,弗吉尼亚州和西弗吉尼亚州,…密西西比州。” 在我的上一篇文章中,我集中于这些州的子集,因为与美国其他地区相比,这些州受糖尿病的影响更大,并且可以进行更集中的分析。 在本文中,我将继续分析此数据并为仅构成糖尿病带的州得出结论。
Before I begin, I want to provide some technical background on this topic. High blood pressure, high cholesterol, and diabetes are all risk factors for heart disease. High blood pressure means that the blood flow in the blood vessels increases, making the heart work more and weakening the heart (American Heart Association, 2016). High levels of cholesterol (a fat found in the body) can occlude blood flow. If blood vessels are occluded with cholesterol, they become narrow and require a much a higher blood pressure to keep blood flowing, eventually weakening the heart and increasing the likelihood of heart disease. Thus, studying the prevalence of these comorbidities is important for population health research.
在开始之前,我想提供有关此主题的一些技术背景。 高血压,高胆固醇和糖尿病都是心脏病的危险因素。 高血压意味着血管中的血流量增加,使心脏更加运转并削弱了心脏(美国心脏协会,2016)。 高水平的胆固醇(体内脂肪)会阻塞血液流动。 如果血管被胆固醇阻塞,血管就会变窄,需要更高的血压才能保持血液流通,最终使心脏虚弱并增加患心脏病的可能性。 因此,研究这些合并症的患病率对于人口健康研究很重要。
Similar to the previous article, I will continue analyzing data for 2017, because it the most recent year with available data.
与上一篇文章类似,我将继续分析2017年的数据,因为它是具有可用数据的最近一年。
First, I want to look at the overall prevalence of diabetes’ comorbidities: high blood pressure and high cholesterol.
首先,我想看看糖尿病合并症的总体患病率:高血压和高胆固醇 。
From the plot above, prevalence of high blood pressure is higher than the prevalence of high cholesterol among adults with diagnosed diabetes. A statistical test confirms that there is a significant difference between the two:
从上图可以看出,在患有糖尿病的成年人中,高血压的患病率高于高胆固醇的患病率。 统计测试确认两者之间存在显着差异:
An independent t-test was used to determine if there were statistically significant differences between prevalence of high blood pressure and prevalence of high cholesterol among adults with diagnosed diabetes. Assumptions for normality (p > 0.05) and homogeneity of variances, using Levene’s Test for Equality of Variances (p > 0.05), were met. For adults with diagnosed diabetes, prevalence of high blood pressure is significantly higher (M = 65.81, SD = 4.81), than prevalence of high cholesterol (M = 56.31, SD = 4.37), p = 0.00 < 0.05.
使用独立的t检验确定在诊断为糖尿病的成年人中高血压患病率与高胆固醇患病率之间是否存在统计学差异。 使用Levene方差均等检验(p> 0.05)满足正态性(p> 0.05)和方差均质性的假设。 对于诊断为糖尿病的成年人,高血压的患病率 (M = 65.81,SD = 4.81) 明显高于 高胆固醇的患病率 (M = 56.31,SD = 4.37),p = 0.00 <0.05。
This observation coincides with data from the CDC’s National Diabetes Statistics Report 2020, which states that 68.4% of adults with diagnosed diabetes had hypertension (blood pressure > 140/90), or were currently prescribed hypertension medications, and 43.5% had high cholesterol levels (LDL cholesterol > 130 mg/dl), from 2013–2016. The prevalence of high blood pressure across the diabetes belt and across the Unites States are similar. However, the prevalence of high cholesterol is higher across the diabetes belt than across the United States. This increase in prevalence of high cholesterol could be attributed to the increased density of adults with diagnosed diabetes in the diabetes belt, compared to the rest of the United States.
该观察结果与CDC的《国家糖尿病统计报告2020》(National Diabetes Statistics Report 2020)的数据相吻合,该报告指出,被诊断为糖尿病的成年人中有68.4%患有高血压(血压> 140/90),或目前正在服用高血压药物,而43.5%的胆固醇水平很高( 2013-2016年,LDL胆固醇> 130 mg / dl)。 整个糖尿病带和整个美国的高血压患病率相似。 但是,在整个糖尿病地区,高胆固醇的患病率高于美国。 与美国其他地区相比,高胆固醇患病率的增加可能归因于在糖尿病带中被诊断为糖尿病的成年人的密度增加。
Next, I want to look at the gender differences between the prevalence of high blood pressure and prevalence of high cholesterol among adults with diagnosed diabetes.
接下来,我想看看诊断为糖尿病的成年人中高血压患病率与高胆固醇患病率之间的性别差异 。
Prevalence of High Blood Pressure among Adults with Diagnosed Diabetes in 2017 2017年诊断为糖尿病的成年人中高血压的患病率Starting with the prevalence of high blood pressure among adults with diagnosed diabetes, I can see that both and male and female adults have a similar prevalence. There is not a significant difference between the two groups, and this is evident through a statistical test:
从诊断出患有糖尿病的成年人中高血压的患病率开始,我可以看到男女成年人和成年人的患病率都相似。 两组之间没有显着差异,这可以通过统计检验来证明:
An independent t-test was used to determine if there were statistically significant differences between prevalence of high blood pressure in males and female adults. Assumptions for normality (p > 0.05) and homogeneity of variances, using Levene’s Test for Equality of Variances (p > 0.05), were met. Prevalence of high blood pressure is not significantly different between males (M = 67.64, SD = 4.90) and females (M = 64.24, SD = 7.15), p = 0.15 > 0.05.
使用独立的t检验来确定男性和女性高血压的患病率之间是否存在统计学上的显着差异。 使用Levene方差均等检验(p> 0.05)满足正态性(p> 0.05)和方差均质性的假设。 男性 (M = 67.64,SD = 4.90) 和女性 (M = 64.24,SD = 7.15) 之间的高血压患病率无显着差异 ,p = 0.15> 0.05。
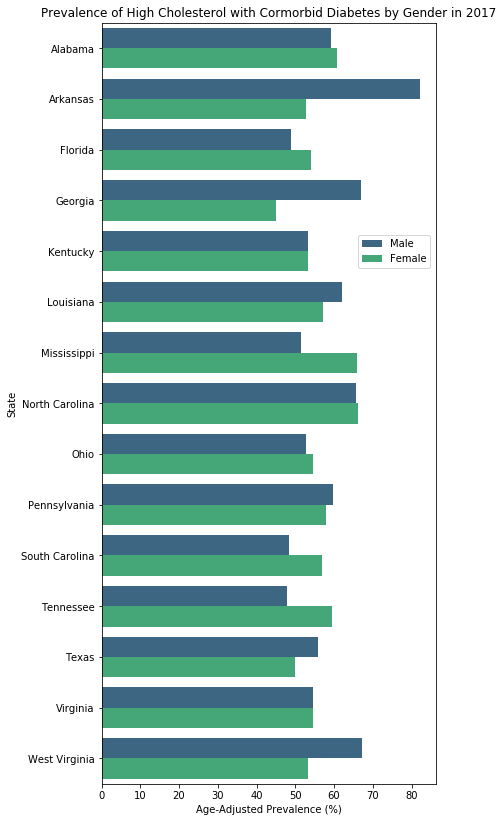
The above plot of prevalence of high cholesterol among adults with diagnosed diabetes shows that both and male and female adults have a similar prevalence of high cholesterol. Statistical tests confirm this:
上面的被诊断患有糖尿病的成年人中高胆固醇的患病率图显示,男女成人和成年人的高胆固醇患病率相似。 统计测试证实了这一点:
An independent t-test was used to determine if there were statistically significant differences between prevalence of high cholesterol in males and female adults. Assumptions for normality (p > 0.05) and homogeneity of variances, using Levene’s Test for Equality of Variances (p > 0.05), were met. Prevalence of high cholesterol is not significantly different between males (M = 58.41, SD = 9.00) and females (M = 56.13, SD = 5.36), p = 0.42 > 0.05.
使用独立的t检验来确定男性和女性成年人中高胆固醇患病率之间是否存在统计学上的显着差异。 使用Levene方差均等检验(p> 0.05)满足正态性(p> 0.05)和方差均质性的假设。 男性 (M = 58.41,SD = 9.00) 和女性 (M = 56.13,SD = 5.36) 之间的高胆固醇患病率无显着差异 ,p = 0.42> 0.05。
The CDI Diabetes dataset also included data on ethnicity; however, I am not considering the role of ethnicity in the prevalence of comorbidities because of the volume of missing data. There is too much data missing for the Black (non-Hispanic) and Hispanic populations for me to make meaningful insights. Nonetheless, I was curious to see what research had been done on the topic of ethnicity differences in diabetes comorbidities. According to Walker et al. (2016), Black (non-Hispanic) individuals “consistently demonstrated the lowest rates of BP [blood pressure] control,” compared to other ethnic groups. Similar trends were seen in lipid control for Black (non-Hispanic) individuals (Walker et al. 2016). In my previous article, an analysis of ethnicity differences showed that Black (non-Hispanic) individuals had the highest diabetes prevalence and diabetes-related mortality rate across the diabetes belt. With Black (non-Hispanic) individuals being highly affected by diabetes; it follows that they would also be highly affected by the comorbidities of diabetes.
CDI糖尿病数据集还包括种族数据。 但是,由于缺少大量数据,我没有考虑种族在合并症流行中的作用。 对于黑人(非西班牙裔)和西班牙裔人口而言,缺少太多数据,我无法做出有意义的见解。 尽管如此,我很好奇,已经对糖尿病合并症的种族差异进行了哪些研究。 据沃克等。 (2016年),与其他族裔群体相比,黑人(非西班牙裔)个体“始终显示出最低的BP(血压)控制率”。 在黑人(非西班牙裔)个体的脂质控制中也观察到类似趋势(Walker等人,2016)。 在我之前的文章中,对种族差异的分析表明,黑人(非西班牙裔)个体在整个糖尿病带中的糖尿病患病率和与糖尿病相关的死亡率最高。 黑人(非西班牙裔)个体受到糖尿病的严重影响; 因此,他们也将受到糖尿病合并症的高度影响。
In my last article, I discussed the limitations of the data. The same limitations apply here. The source of this data is Behavioral Risk Factor Surveillance System (BRFFS), which collects data through surveys and provides data for adults with diagnosed diabetes. Thus, anyone that is not reached through the BRFFS’s survey collection methodology is not included, nor are individuals with undiagnosed diabetes. Further, there is no distinction between Type 1 and Type 2 diabetes.
在上一篇文章中,我讨论了数据的局限性。 同样的限制在这里适用。 该数据的来源是行为风险因素监视系统(BRFFS),该系统通过调查收集数据,并为诊断为糖尿病的成年人提供数据。 因此,不包括通过BRFFS的调查收集方法无法获得的任何人,也不会包括没有被诊断为糖尿病的人。 此外,在1型和2型糖尿病之间没有区别。
Another limitation is that the data for ethnicity is missing for these two particular questions in the CDI Diabetes dataset. Gender, ethnicity, environmental factors, and sociocultural factors all contribute to diabetes development; therefore, it is difficult to put together a picture without all the pieces.
另一个限制是CDI糖尿病数据集中的这两个特定问题缺少种族数据。 性别,种族,环境因素和社会文化因素均会导致糖尿病的发展; 因此,很难将所有内容都拼凑在一起。
In conclusion, diabetes is a complex disease, with numerous risk factors and complications. My analysis of the CDI Diabetes dataset looks at how high blood pressure, high cholesterol, and diabetes are linked to each other. In this dataset, there is no sex bias for either high blood pressure or high cholesterol among adults with diagnosed diabetes, but there is a significantly higher prevalence of high blood pressure than high cholesterol among adults with diagnosed diabetes in the diabetes belt in 2017.
总之,糖尿病是一种复杂的疾病,具有许多危险因素和并发症。 我对CDI糖尿病数据集的分析着眼于高血压,高胆固醇和糖尿病之间的相互联系。 在该数据集中,在诊断为糖尿病的成年人中,高血压或高胆固醇均无性别偏见,但2017年在糖尿病带中,在诊断为糖尿病的成年人中,高血压的患病率明显高于高胆固醇。
引文: (Citations:)
American Heart Association. “How High Blood Pressure Can Lead to Heart Failure.” 2016, https://www.heart.org/en/health-topics/high-blood-pressure/health-threats-from-high-blood-pressure/how-high-blood-pressure-can-lead-to-heart-failure
美国心脏协会。 “高血压如何导致心力衰竭。” 2016年, https://www.heart.org/en/health-topics/high-blood-pressure/health-threats-from-high-blood-pressure/how-high-blood-pressure-can-lead-to-心脏衰竭
Barker, Lawrence E et al. “Geographic distribution of diagnosed diabetes in the U.S.: a diabetes belt.” American journal of preventive medicine vol. 40,4 (2011): 434–9. doi:10.1016/j.amepre.2010.12.019
Barker,Lawrence E等。 “在美国诊断出的糖尿病的地理分布:糖尿病带。” 美国预防医学杂志。 40,4(2011):434–9。 doi:10.1016 / j.amepre.2010.12.019
Centers for Disease Control and Prevention, National Diabetes Statistics Report 2020. Page 9. “Risk Factors for Diabetes Related Complications”. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
疾病控制和预防中心,《 2020年全国糖尿病统计报告》。第9页。“糖尿病相关并发症的风险因素”。 https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf
Walker, Rebekah J et al. “Influence of Race, Ethnicity and Social Determinants of Health on Diabetes Outcomes.” The American journal of the medical sciences vol. 351,4 (2016): 366–73. doi:10.1016/j.amjms.2016.01.008
沃克,丽贝卡J等。 “种族,种族和健康的社会决定因素对糖尿病结局的影响。” 美国医学杂志第一卷。 351,4(2016):366–73。 doi:10.1016 / j.amjms.2016.01.008
翻译自: https://towardsdatascience.com/exploring-the-relationship-between-diabetes-high-blood-pressure-and-high-cholesterol-in-the-cdi-16f15fc80b73
胆固醇偏高会影响入职