本科毕业设计(论文)外文翻译--采用多病人协调器集设计方法的远程温度监测装置
英文原文
起止页码:1-13
Remote temperature monitoring device using a
multiple patients-coordinator set design approach
Abstract
This paper aims to develop a prototype for a web-based wireless remote temperature monitoring device for patients. This device uses a patient and coordinator set design approach involving the measurement, transmission,receipt and recording of patients’ temperatures via the MiWi wireless network. The results of experimental tests on the proposed system indicated a wider distance coverage and reasonable temperature resolution and standard deviation. The system could display the temperature and patient information remotely via a graphical-user interface as shown in the tests on three healthy participants. By continuously monitoring participants’ temperatures, this device will likely improve the quality of the health care of the patients in normal ward as less human workload is involved.
Keywords: Temperature; Wireless; Web-based; Remote; Monitoring; Patient set; Coordinator set
Background
During the severe acute respiratory syndrome (SARS) outbreak in 2003, hospitals became treatment centres in most countries. Because a patient’s core body temperature is one vital parameter for monitoring the progress of the patient’s health, it is often measured manually at a frequency ranging from once every few hours to once a day [1]. However, such manual measurement of the temperature of patients requires the efforts of many staff members. In addition, when the patients suffer from
conditions that result in abrupt changes of the core body temperature, e.g., due to infection at a surgical site after surgery, the staff on duty will not know such a temperature change occurred until the next temperature measurement. Such a delay may lead to patients being unnoticed while their health conditions worsen, which is dangerous because a difference of 1.5 degrees Celsius can result in adverse outcomes [2]. Furthermore, there is always a need to have a monitoring system to improve
the quality of health care [3], such as temperature monitoring of elderly and challenged persons using a wireless remote temperature monitoring system.
Body temperature can be used to monitor the pain level of a patient following an operation [4] or after shoulder endoprosthesis [5]. In some cases, the tissue transient temperature was monitored during microwave liver ablation [6] for the treatment of liver metastases. Instead of using a temperature sensor, pulse-echo ultrasound [7] was used to visualize changes in the temperature of the patient’s body. In addition, a non-contact temperature-measuring device, such as a thermal imaging camera [8], was successfully used to detect human body temperature during the SARS outbreak. However, it can be quite expensive to equip each patient room with a thermal imaging camera. In addition, there are a few wireless temperature-monitoring systems (e.g.,CADIT™, Primex™, and TempTrak™) on the market that are used to monitor and store a patient’s temperature for medical research by using body sensor networks [9].Most of these systems consist of an electronic module and a temperature-sensing device. The systems include a stand-alone electronic module with a display screen that allows the temperature sensor data to be transmitted over a secure wireless network.
However, these systems can be difficult to reconfigure to suit the current database system used in the hospital.In addition, the current systems using short message service (SMS)-based telemedicine [10] systems with hardware equipment were developed to monitor the mobility of patients. However, proper hardware and software to manage the messages and the patient’s temperature for display on mobile phones are not widely available.
Hence, a medical device to continuously measure the body temperature of patients using a wireless temperature sensor [4,11,12] is required. With such a wireless temperature sensor system, nurses will no longer have to manually measure the temperature of patients, which will free their time for other tasks and also reduce the risk associated with coming into contact with patients with contagious diseases, such as SARS. The readings will be transmitted wirelessly to the central nurse station, where they can be monitored by the staff-on-duty.In addition, the current and past history of the body temperature measurements can be stored in an online database, which allows the medical staff to access the database when they are not in the hospital.
To the best of our knowledge, a MiWi wireless (besides using the Zigbee[11]) temperature-monitoring system using a patient and coordinator set design that provides remote internet access to the temperature database has not been reported in any publication. The objective is therefore to develop and implement a prototype temperature-monitoring system for patients using a MiWi wireless remote connection to the nurse’s station for frequent real-time monitoring. The temperature monitoring system was designed based on a proposed patient and coordinator set design approach. The proposed temperature-monitoring system for use in normal ward will likely to improve the quality of the health care of the patients as the nursing workload is reduced. In this paper, the discussion on medical regulations and policy will not be included.
Method
Design concepts of the wireless remote temperaturemonitoring system
The core body temperature of a human is one of the vital statistics used to determine individual health. Normal human body temperature (normothermia) is approximately 37°C, with variations depending on factors such as age and geological factor [13]. When the body fails to regulate itself by dissipating heat, it increases the core body temperature above the normal condition.
This condition is called hyperthermia. The highest recorded surviving core body temperature is 45°C [14].Generally, there are four locations [15] that can be used to measure human core body temperature, rectal (anus),oral (mouth), tympanic (ear) and axillary (armpit), with the rectal measurement considered to be the most accurate in measuring the core body temperature. Rectal measurement of body temperature is the preferred method to perform a core body temperature measurement.In order to track a patient’s core body temperature wirelessly (assuming the patient is not moving), the axillary measurement was chosen for the initial trial. The proposed measurement system must be able to measure within the temperature deviation [16,17] of 0.3-0.5°C and detect changes in the human body temperature (at minimum resolution of 0.1°C).
MiWi wireless network
The originality of the paper is to develop and test a prototype temperature-monitoring system for patients using the MiWi wireless remote connection to the nurse’s station for frequent real-time monitoring. As this project aims to be implemented in a hospital environment, when choosing the appropriate wireless technology it should be noted that the chosen technology should be the best choice in terms of cost, connectivity range, speed, etc. for the chosen environment. Table 1 below depicts the comparison between ZigBee, Bluetooth and Wi-Fi.
It is concluded from the table that ZigBee is the most fitting technology for this project. The main reason for this decision is because ZigBee requires very low power consumption by staying on sleep mode most of the time while still having the same range potential as Bluetooth and Wi-Fi. Another advantage of using ZigBee comes from having more possible topology which is star that allows 1 FFD (Full Function Device) unit to control multiple RFD (Reduced Function Device) units and mesh which allows the system to be more resistant to RFD unit breaking down as can be seen on Figure 1. While
Table 1 Wireless technologies comparison
Fig.1 Different ZigBee topologies
ZigBee has lower data rate than the other two, it is sufficient for transmitting the temperature data that will be measured in this project.
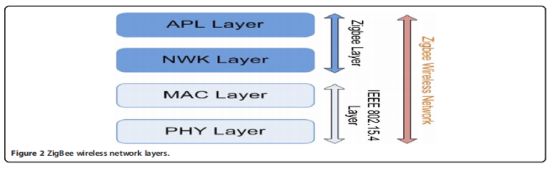
ZigBee’s is mostly used in low power, low data rate application such as home monitoring system due to its benefits compared to other wireless technologies as explained in Table 1. Each device can be configured into two different types: FFD which can communicate with both types and RFD which can only communicate with FFD type. FFD can be configured into a coordinator which is the base station in this project, or router which serves to extend the range of the system. FFD is configured as patient’s unit in this project. The ZigBee network itself works in layers as shown in Figure 2 with each having specific task to manage the wireless connection. The PHY (physical) layer manages data transmission by performing quality checking on both channel frequency and in/outgoing signals and also managing the RF transceiver module. Some of the specific tasks it needs to do are energy detection, link quality indication, clear channel assessment and channel selection. The MAC (Media Access Control) layer manages the access of data into the frequency channel and control the network beaconing. It also assigns time slots for the transmitted data and manages data security. The NWK (network) layer manages the whole network connectivity by doing tasks such as ensuring the MAC layer is used correctly and identifying whether a neighbouring device belongs to the system or not. The NWK layer is also responsible for creating a suitable interface for highest APL (application)layer in which the users can interact with the ZigBee application and interface.
Unfortunately, the ZigBee protocol stack is too large for most commonly used MCUs’ memory to handle. Therefore MiWi protocol stack will be used instead.MiWi wireless transceiver (MRF24J40MA) used in the project support P2P protocol. There is no significant different from other P2P protocols. But when compared with the ZigBee protocol stack, ZigBee protocol is too large for most commonly used MCUs’ memory to handle. The reason is that MiWi protocol stack only uses the MAC and PHY layers which reduce the code used.Another merits using MiWi P2P are the protocol is proprietary and it is not interoperable. In addition, MiWi P2P has also a small footprint and a very low overhead as compared with ZigBee protocol. However, the demerits of MiWi P2P are the small network size and only allow small number of hops.
Fig.2 ZigBee wireless network layers
When compared to grid networks which provide many servers to moderate-sized communities and emphasize the integration of resources to deliver in an environment of at least limited trust, P2P deal with many more participants but offer limited and specialized servers, have been less concerned with qualities of service, and limited assumptions about trust. But as system scale increases in the grid networks, it may face and address problems relating to autonomic configuration and management. On the other hand, the P2P developed rapidly around sharing and are now seeking to expand to more sophisticated applications and management.
Multiple patients-coordinator set design approach
To accomplish the axillary temperature measurement, the wireless remote temperature monitoring system design (see Figure 3) includes a MiWi wireless transceiver (MRF24J40MA), a PIC microprocessor (PIC18LF4620)/MCU, a temperature sensing circuit, a patient set (on the patients) and a coordinator set (at the nurse’s station) for the data coordination between the patients and the central nurse station. The temperature sensor produced an output voltage (and power consumption of 0.24 mW) with a magnitude equal to the body temperature. The analogue-to-digital convertor (ADC) had 13 analogue channels and a 10-bit resolution in the microprocessor to convert the output voltage into digital values. The patient’s transceiver transmitted that digital value via the MiWi wireless protocol stack to the coordinator’s transceiver. The coordinator MCU sent the temperature reading to the computer through RS232 that records and stored the temperature measurements in the database. The proposed wireless temperature-monitoring device could support multiple patients when they were connected to the same wireless network.There are a few wireless and wired temperature sensors available to monitor the temperature of patients.The temperature resolution is approximately +/-0.2°C for the range 25-60°C. However, a 1.5°C loss [2] in body temperature, e.g., due to surgical site infection after surgery, may lead to adverse outcomes. Hence, a resolution of +/- 0.1°C is required. Because the highest recorded surviving core body temperature is 45°C, the temperature range required for the temperature sensor is reduced. For initial prototyping, a non-medical-grade LM35CAZ temperature sensor with a maximum range of 45°C was used. The temperature sensor used draws only 60 μA from its supply and power consumption is approximately 0.24 mW. The following is the specifications of the LM35CAZ temperature sensor.
Calibrated Directly in ° Celsius (Centigrade)
Linear + 10 mV/°C Scale Factor
0.5°C Ensured Accuracy (at +25°C)
Rated for Full −55°C to +150°C Range
Operates from 4 to 30 V
Less than 60-μA Current Drain
Low Self-Heating, 0.08°C in Still Air
Low Impedance Output, 0.1 Ω for 1 mA Load
Thus, the only advantage compared to the medicalgrade sensor is the low power consumption. Nevertheless,the sensor can be replaced with any medical-grade temperature probe (such as a standard stick-on skin probe) with minor changes in the hardware and software.
Fig.3 Overall block diagram of the multients-coordinator set design approach
Patient set design
The patient set consists of three main components: temperature sensor circuit, MCU and transceiver. The electronic components were mounted onto a small PCB board and connected to the patient’s MCU. As shown in Figure 4, the setup (within the enclosure) was strapped to the patient’s arm during temperature monitoring.
Initially, only two patient sets were used. When the patient MCU was turned on, it established a connection with the coordinator set using a wireless protocol stack. For the initial phase of the project, the easy-to-use alternative for simple wireless communication of MiWi (by MicroChip) was used to implement the low-cost and power wireless control networks (with a battery usage of 95-115 μW compared with ZigBee at approximately 30 mW).A MiWi wireless transceiver module (MRF24J40MA-2.5GHz IEEE 802.15.4) was mounted onto a carrier board.To allow easy configuration and to monitor packet transactions, a ZENA wireless network analyser (DM183023)and software were used. Figure 5 (top) shows an example of a transmitted message viewed on the ZENA network analyser. The first line indicates the patient node attempting to join a network, while the second line indicates the coordinator recognizing the patient node as a member of the network.
Because the ADC has 10 bits, the output was separated into two registers (two bytes). The 2-byte digital output values were sent to the coordinator set with an additional byte to indicate which patient set sent the data. Sometimes, there may be a disruption or glitch in the MiWi wireless network that prevents the coordinator from receiving the data from the patient. To overcome this issue, a cyclic redundancy check (CRC) of 16 bits (or 2 bytes in length) was used to determine whether the packet was correctly transmitted. For example,if the entire set of bits was correct, the CRC value matched. FCS had the OK bit in the last byte of the data.However, if a single bit was incorrect, the data need to be retran smitted.
The patient set temperature conversion process from the temperature sensor is as follows. The temperature sensor of Patient Set 1 produced an output voltage of 0.365 V or 36.5°C. This voltage was amplified 5.12 times to 1.868 V. The ADC converted the voltage into two registers of 1 byte each (conversion to hexadecimal) to obtain 02 46. Subsequently, the MCU added an additional byte to identify the patient set. If Patient Set 1 was used, the extra byte was 01. Subsequently, the transceiver transmitted the 3 bytes to the coordinator MCU and displayed the temperature on the computer with the GUI.
Coordinator set design
As shown in Figure 5 (centre), the coordinator set requires a similar MCU and transceiver in the patient set.Each patient set was designed to send a message of 3 bytes to the coordinator MCU. The coordinator’s MCU performs a few tasks, as shown in the flow chart. The tasks was to establish a connection with each patient set, send an acknowledgement byte to the patient set after receiving the message, and send the message to the coordinator. The GUI of the coordinator set created a text file containing the temperature reading for a day. The file was stored in the local PC folder with all of the temperature data, the patients’ name (with serial or patient number) and the time stamps. The graphical representation of the temperature distribution of the patient is shown in Figure 5. Statistical information,such as the mean and standard deviation for certain time frame, was then computed. The information was displayed on the staff computer near the coordinator patient set.
Patient and coordinator set wireless transmission tests
The hardware setup in the laboratory consists of the temperature sensor, amplifier circuit, coordinator MCU and patient MCU, as shown in Figure 4 (right). The output voltage was calibrated and compared with a digital
Fig.4 Prototype temperature-monitoring system strapped on patient set 1(left)and circuit board (right)
Fig.5 ZENA wireless network analyser output(top),GUI for the coordinator set(center) and online database at the
thermometer (i.e. OMRON™ digital thermometer) reading for a few times. It was observed that the sensor output voltage would yield a tolerance level of ±0.2°C when compared with the thermometer readings. In addition,the amplifier circuit had an input voltage of 307.4 mV that was amplified 5.12 times to 1.573 V and displays the result of the ADC process in the ZENA network analyser. The ADC converted the input voltage to the hexadecimal corresponding to 20.3°C, as shown in Figure 5(top). The test indicated that the ADC conversion process in the patient’s MCU was able to measure the temperature correctly.
As mentioned, the patient MCU sent the 3-byte message to the coordinator MCU. To test this feature, the patient set transmitted the message every few seconds to the coordinator to process the message. The coordinator MCU sent an acknowledgement message until the CRC was shown positive. As shown in Figure 5 (top), an additional patient has the first byte of its message changed to differentiate between different patients. Figure 5 also shows that the coordinator (source address ending with01 at the payload section) was able to receive messages from multiple patients.
The network coverage range of the MRF24J40MA transceiver was conducted in a school campus to test the network coverage range. The coordinator MCU was placed in a room, while a patient MCU was along the corridor. The coordinator MCU sent a message every few seconds. The signal could be transmitted with a clear line of sight to a distance of approximately 50 m.In addition to testing the indoor network coverage, the range of 120 meters provided in the datasheet was validated in a test outdoors at an ambient temperature of 26°C.
Results
Actual implementation of the proposed system on patients
The proposed wireless remote temperature monitoring device was tested on three healthy participants at a classroom (with computers) in the school environment for three different days. We took their temperature when they were sitting during the experiment. The sensor was attached to the body during the measurement only. They took the sensor off when they wanted to relax and lay on foldable beds.
The authors had received the ethics approvals and informed consent from the three participants before the tests were conducted.
The GUI of the coordinator set (for the nurse’s station) in Figure 5 (centre) was used. The coordinator set was connected to the coordinator computer via the RS-232 serial cable. Each time the coordinator MCU received a temperature reading message, it sent the message to the coordinator’s computer. Upon clicking on the ‘Update Chart’ button, the GUI read and generated the temperature record chart for that particular patient and date. Once the message was received, the GUI converted the inputs to actual temperature reading.
The user can allocate a patient name tagged with his/her admission serial number. Once allocated, the patient name with the serial number was applied to the local folder in the database. Figure 5 (bottom) shows the local temperature record of a subject. The temperature record was saved in the text file, and the data were formatted as“Temperature-Time”.
In the nurse’s station, the two main components used in the implementation of the online database were the MySQL database and the PHP scripts. An online hosting server called sparkstation.net was used. Each set of patient information includes the temperature, time, and date created by the coordinator. To operate the system properly, the users were trained to retrieve and provide the correct patient information. There was an added feature of using different colours to indicate the patients with high fever; in addition, in the event of a large standard deviation (or equivalent to a sharp slope), an alarm would be triggered.
Statistical information, such as the mean and the standard deviation, for evaluating the data variation was determined. For an initial trial, 20 minutes of recording and sampling at an interval of 2 minutes was conducted to test the proposed system. The subsequent temperature recording was sampled or taken in every hour. The mean of the participant temperature was 36.6 (95% confidence intervals of 35.9 and 37.3). The standard deviation was 1.0 (95% confidence intervals of 0.7 and 1.8),and the median was 36.9 (95% confidence intervals of 36.0 and 37.2).
The wireless remote temperature monitoring system was tested in three different days (named D1, D2 and D3) on three healthy male participants (named P1, P2 and P3) with ages ranging from 28 to 30 years. The interval between each measurement was set to one hour,starting at 1 am. The body temperatures of the three participants were recorded and plotted on a time series plot,as shown in Figure 6. The statistical mean temperatures for P1, P2, and P3 on different days were 36.8°C, 36.7°C, and 37.8°C, respectively, and the statistical standard deviations for P1, P2, and P3 were approximately 0.3°C. These values were computed using the temperature data collected over 24 hour.
As seen in Figure 6, the wireless remote temperature monitoring system was able to measure the temperatures of the participants from 1st to 24th hour. The highest
Fig.6 Temperature of three different participants over three days
standard deviation was approximately 0.3°C, which is within the range of 0.3 to 0.5°C [16,17] in an enclosed building environment throughout the test period. In summary, the proposed system could measure body temperature within the resolution of 0.3 to 0.5°C and exhibit small standard deviation of 0.3°C.
Discussions
The temperature readings of the participants who wore the portable temperature monitoring devices were transmitted wirelessly to the main station where they were monitored. The body temperature measurements were stored in an online database, which allowed the user to access the database when they were not with the participants.
The target patients using the device are for those in the normal wards instead of intensive care unit (ICU).Although the monitoring once a day is enough to detect the adverse or other problems because the nurses go around the normal wards to see the patients, the proposed device helps to free their time for other tasks and also reduce the risk associated with coming into contact with patients with contagious diseases. With the help of the device, it offers an added precautionary measure to ensure adequate temperature monitoring for all patients in the normal ward are done with minimal effort. During the tests on the three participants in different days, we observed that the P1 and P2 had a higher temperature than P3 in particular on the Day 3. That might be due to some “exhaustion” after 2 days. We did suspect the temperature sensor problem but when we calibrated the temperature against the thermometer, it was fine. The reason for no trend in the temperature reason (such as having the circadian rhythm [18]) is due to the participants was actually quite awake (for example, they were chatting and playing with their smart phones) and they did not really fall into sleep.
Conclusions
This paper presents a web-based MiWi wireless remote temperature-monitoring device using temperature sensors for the axillary measurement. The temperature data were sent via the MiWi wireless protocol to the nurse’s station connected to internet. This approach was facilitated by a patient and coordinator set design that connects the process of monitoring, transmitting, alerting and recording of the temperature. The experimental tests on the proposed device indicated that it provides long-distance coverage, a temperature resolution of 0.3 to 0.5°C and small standard deviation of approximately 0.3°C. Importantly, the system will likely to improve the quality of care through 24-hour continuous monitoring of the temperature of patients and reducing the workload of the nursing staff in normal ward.
The remote temperature monitoring device will be further developed into a low-cost product with plug-andplay feature that enable untrained nurse or doctors to use with minimal assistance. The software interface for users will be improved and made easy to be installed and downloaded. For future work involving remote monitoring, the use of different wireless network protocols, such as ZigBee and WiFi, will be compared. A standard medical temperature probe, such as a tympanic probe, and standard disposable tape will be used for final implementation in the hospital. Further evaluation of the proposed system against current measurement techniques needs to be performed. The privacy and security protection and export to clinical information system(CIS) will be studied.
- 中文译文
采用多病人协调器集设计方法的远程温度监测装置
摘要:本文旨在研制一种基于网络的无线病人远程温度监测装置。该设备使用患者和协调员集设计方法,包括通过MIWI无线网络测量、传输、接收和记录患者的温度。实验结果表明,该系统覆盖范围广,温度分辨率和标准偏差合理。该系统可以通过一个图形用户界面远程显示温度和患者信息,如三名健康参与者的测试所示。通过持续监测受试者的体温,该设备将有可能提高正常病房患者的医疗质量,因为所涉及的人力工作量较少。
关键词:温度;无线;基于网络;远程;监控;患者设置;协调员设置
背景:在2003年严重急性呼吸综合征(SARS)爆发期间,医院成为大多数国家的治疗中心。由于患者的核心体温是监测患者健康进展的一个重要参数,因此通常以每几个小时一次到每天一次的频率手动测量体温[1]。然而,这种对病人体温的手动测量需要许多工作人员的努力。此外,当患者出现导致核心体温突然变化的情况时,例如由于手术后手术部位感染,值班人员直到下一次温度测量时才会知道发生了这种体温变化。这种延迟可能会导致患者在健康状况恶化时被忽视,这是危险的,因为1.5摄氏度的差异可能会导致不良后果[2]。此外,始终需要有一个监测系统来提高医疗质量[3],例如使用无线远程温度监测系统监测老年人和受挑战者的温度。
体温可用于监测患者术后或肩关节假体术后的疼痛程度[4]。在某些情况下,在微波肝消融[6]治疗肝转移过程中监测组织瞬时温度。而不是使用温度传感器,脉冲回波超声波[7]是用来可视化的变化,病人的身体温度。此外,一种非接触式温度测量装置,如热成像摄像机[8],成功地用于在非典爆发期间检测人体温度。但是,为每个病房配备一台热成像摄像机可能会非常昂贵。此外,市场上还有一些无线温度监测系统(例如cadit™、primex™和tentrak™)用于通过人体传感器网络监测和存储患者的体温,以供医学研究[9]。大多数这些系统由电子模块和温度传感设备组成。该系统包括一个带有显示屏的独立电子模块,该显示屏允许通过安全无线网络传输温度传感器数据。
然而,这些系统很难重新配置,以适应当前医院使用的数据库系统。此外,目前的系统使用基于短消息服务(SMS)的远程医疗[10]系统和硬件设备来监控患者的移动。然而,用于管理信息的适当硬件和软件以及用于在移动电话上显示的患者温度并不是广泛可用的。
因此,需要使用无线温度传感器[4、11、12]连续测量患者体温的医疗设备。有了这样一个无线温度传感器系统,护士将不再需要手动测量病人的温度,这将为其他任务腾出时间,并降低与传染性疾病(如非典)病人接触的风险。这些读数将无线传输到中央护士站,由值班人员监控。此外,体温测量的当前和过去的历史记录可存储在在线数据库中,允许医务人员在不在医院时访问数据库。
据我们所知,MIWI无线(除使用ZigBee[11]外)温度监测系统采用患者和协调器组设计,提供远程互联网访问温度数据库,在任何出版物中均未报告。因此,我们的目标是开发和实现一个原型温度监测系统,该系统使用MIWI无线远程连接到护士站,以便进行频繁的实时监测。温度监测系统的设计是基于一个拟议的病人和协调员集设计方法。随着护理工作量的减少,推荐的用于普通病房的温度监测系统有可能提高患者的医疗质量。本文不讨论医疗法规和政策。
方法:无线远程温度监测系统的设计思想
人体核心体温是用来确定个人健康状况的重要统计数据之一。人体正常体温(常温)约为37°C,随年龄和地质因素等因素而变化[13]。当身体不能通过散热来自我调节时,它会使核心体温高于正常体温。
这种情况称为热疗。记录的最高存活核心体温为45°C[14],一般有四个位置[15]可用于测量人体核心体温:直肠(肛门)、口腔(口)、鼓室(耳)和腋窝(腋窝),直肠测量被认为是测量核心体温最准确的位置。直肠体温测量是进行核心体温测量的首选方法。为了无线跟踪患者的核心体温(假设患者没有移动),在初始试验中选择了腋下测量。建议的测量系统必须能够在0.3-0.5°C的温度偏差[16,17]范围内进行测量,并检测人体温度的变化(最低分辨率为0.1°C)。
1、MIWI无线网络
本文的初衷是利用MIWI无线远程连接护士站,开发并测试一个病人温度监测系统的原型,实现对病人的频繁实时监测。由于本项目的目标是在医院环境中实施,因此在选择适当的无线技术时,应注意所选技术在成本、连接范围、速度等方面应是所选环境的最佳选择。下表1描述了ZigBee、蓝牙和Wi-Fi之间的比较。
从表中可以看出,ZigBee是本项目最合适的技术。这一决定的主要原因是,ZigBee需要非常低的功耗,因为大部分时间保持睡眠模式,同时仍具有与蓝牙和Wi-Fi相同的范围潜力。使用ZigBee的另一个优点是具有更多可能的拓扑结构,即Star,它允许1个FFD(全功能设备)单元控制多个RFD(简化功能设备)单元和网格,使系统能够更抵抗RFD单元分解,如图1所示。虽然ZigBee的数据传输速率比其他两个数据传输速率低,但它足以传输本项目中测量的温度数据。
ZigBee主要用于低功耗、低数据速率的应用,如家庭监控系统,这是因为与表1中所述的其他无线技术相比,ZigBee具有优势。每个设备可以配置为两种不同的类型:可以与两种类型通信的FFD和只能与FFD类型通信的RFD。可将FFD配置为协调器(本项目中的基站)或路由器(用于扩展系统范围)。在这个项目中,FFD被配置为患者的单位。ZigBee网络本身按图2所示分层工作,每个层都有特定的任务来管理无线连接。物理层通过对通道频率和输入/输出信号进行质量检查以及管理射频收发器模块来管理数据传输。它需要做的一些具体任务是能量检测、链路质量指示、清晰的信道评估和信道选择。MAC(媒体访问控制)层管理进入频率通道的数据访问,并控制网络信标。它还为传输的数据分配时隙并管理数据安全。nwk(网络)层通过执行诸如确保正确使用MAC层以及标识相邻设备是否属于系统等任务来管理整个网络连接。nwk层还负责为最高的apl(应用程序)层创建合适的接口,用户可以在其中与zigbee应用程序和接口交互。
不幸的是,ZigBee协议栈太大,大多数常用的MCU内存无法处理。因此,将使用MIWI协议栈代替。项目中使用的MIWI无线收发器(MRF24J40MA)支持P2P协议。与其他P2P协议没有显著差异。但是与ZigBee协议栈相比,ZigBee协议太大,大多数常用的MCU内存无法处理。其原因是MIWI协议栈只使用减少所用代码的MAC和PHY层,而使用MIWI P2P协议的另一个优点是协议是专有的,不可互操作。此外,与ZigBee协议相比,MIWIP2P的占地面积小,开销也很低。然而,miwi p2p的缺点是网络规模小,只允许少量的跃点。与向中等规模的社区提供多台服务器并强调在至少有限信任的环境中整合资源的网格网络相比,p2p处理的参与者更多,但提供的资源有限且具体。而对于服务质量的关注较少,对信任的假设也有限。但是,随着网格网络中系统规模的增加,它可能面临并解决与自主配置和管理相关的问题。另一方面,P2P围绕共享迅速发展,现在正寻求扩展到更复杂的应用程序和管理。
2、多患者协调器集设计方法
为了完成腋窝温度测量,无线远程温度监测系统设计(见图3)包括一个MIWI无线收发器(MRF24J40MA)、一个PIC微处理器(PIC18LF4620)/MCU、一个温度传感电路、一个病人组(在病人身上)和一个用于数据协调的协调器组(在护士站)。病人和中心护士站之间的联系。温度传感器产生输出电压(和0.24 mW的功耗),其大小等于车身温度。模拟数字转换器(ADC)在微处理器中有13个模拟通道和10位分辨率,用于将输出电压转换为数字值。患者的收发器通过MIWI无线协议栈将该数字值传输到协调员的收发器。协调单片机通过RS232将温度读数发送到计算机,并将温度测量值记录和存储在数据库中。所提议的无线温度监测装置可在多个患者连接到同一无线网络时支持多个患者。有一些无线和有线温度传感器可用于监测患者的温度。在25-60°C范围内,温度分辨率约为+/-0.2°C。但是,在体温,例如术后手术部位感染,可能导致不良后果。因此,要求分辨率为+/-0.1°C。由于记录的最高存活堆芯体温度为45°C,因此温度传感器所需的温度范围减小。对于初始原型,使用最大范围为45°C的非医用级LM35CAZ温度传感器。所用的温度传感器仅从其电源中抽取60μA,功耗约为0.24 mW。以下是LM35CAZ温度传感器的规格。
直接以摄氏度(摄氏度)校准
线性+10 mV/°C标度因数
0.5°C保证精度(在+25°C时)
额定全-55°C至+150°C范围
工作电压从4到30 V
小于60μA的电流漏极
低自热,静止空气中0.08°C
低阻抗输出,1 mA负载为0.1Ω
因此,与MedicalGrade传感器相比,唯一的优势是功耗低。然而,传感器可以替换为任何医用级温度探头(如标准贴装式皮肤探头),硬件和软件都会有细微的变化。
3、患者组设计
患者仪主要由三部分组成:温度传感器电路、单片机和收发器。电子元件被安装在一个小的印刷电路板上,并连接到病人的微控制器上。如图4所示,在温度监测期间,将设置(在外壳内)绑在患者手臂上。
最初,只使用了两组患者。当患者的MCU打开时,它使用无线协议栈与协调器集建立了连接。在项目的初始阶段,采用易于使用的MIWI简单无线通信替代方案(通过微芯片)来实现低成本和高功率的无线控制网络(电池使用率为95-115μW,而ZigBee的电池使用率约为30 mW),MIWI无线收发器模块(MRF24J40MA-2.5GHz,IEEE 802.15.4)为M。安装在一个载波板上。为了便于配置和监控数据包事务,使用了Zena无线网络分析仪(DM183023)和软件。图5(顶部)显示了在Zena网络分析仪上查看的传输消息的示例。第一行指示尝试加入网络的患者节点,而第二行指示协调员将患者节点识别为网络成员。
因为ADC有10位,所以输出被分成两个寄存器(两个字节)。2字节的数字输出值与一个额外的字节一起发送给协调器集,以指示哪个患者集发送了数据。有时,MIWI无线网络可能会出现中断或故障,从而阻止协调员接收患者的数据。为了克服这个问题,使用16位(或2字节长)的循环冗余校验(CRC)来确定数据包是否正确传输。例如,如果整组位正确,则CRC值匹配。未来作战系统在数据的最后一个字节中有OK位,但如果一个位不正确,则需要重新传输数据。
温度传感器的患者设定温度转换过程如下。患者组1的温度传感器产生0.365 V或36.5°C的输出电压。该电压被放大5.12倍至1.868 V。ADC将电压转换为两个寄存器,每个寄存器1字节(转换为十六进制),以获得02 46。随后,MCU添加了一个额外的字节来标识患者集。如果使用病人组1,则额外字节为01。随后,收发器将3个字节传输到协调器MCU,并用图形用户界面在计算机上显示温度。
4、集设计协调员
作为显示在图5(中心),需要一个类似的等效集单片机和收发器的病人设计的集集。每个病人所发送的消息的字节单片机3的协调员。漫游协调员的MCU执行一些任务,如显示在流程图。的任务是建立一个集连接病人,病人acknowledgement发送字节集接收到消息后,发送消息到协调员。在GUI的协调员集创建的文本文件阅读节包含一个温度。什么是存储在本地文件的文件夹的所有PC机的温度数据,病人的名字(与串行或病人数)和时间邮票。的温度分布的图形表示显示在图5的病人。统计信息,如均值和标准差的时间是特定的帧,然后计算。位置信息显示在计算机的什么位置靠近协调员病人集。
5、患者和协调员设置无线传输测试
实验室硬件设置包括温度传感器、放大器电路、协调单片机和病人单片机,如图4(右)所示。校准输出电压,并将其与数字温度计(即OMRON™数字温度计)读数进行几次比较。观察到,与温度计读数相比,传感器输出电压将产生±0.2°C的公差水平。此外,放大器电路的输入电压为307.4 mV,放大5.12倍至1.573 V,并在Zena网络分析仪中显示ADC过程的结果。ADC将输入电压转换为对应于20.3°C的十六进制,如图5(顶部)所示。实验结果表明,患者单片机中的ADC转换过程能够正确测量温度。
如上述,《晚期病人单片机的3字节的消息的coordinator单片机。这两个试验的患者的特征,该消息传来说每几秒的两个coordinator处理该消息。《晚coordinator单片机的CRC acknowledgement消息直到shown是积极的。在图5 shown AA(上),一个额外的病人有由其第一字节的消息了differentiate之间的两个不同的病人。图5显示,也coordinator(源地址with01结局的有效载荷部分)是能够接收信息从多的病人。
网络覆盖范围的传导mrf24j40ma收发信机是在一个中学校园内的两个测试网络的覆盖范围。《coordinator placed单片机是在一个房间里,当一个病人的单片机是沿着走廊。《单片机coordinator晚一些消息的每一秒。我可以是传《信号与一个清晰的线的视线的一部约50米的距离。在添加测试的室内网络覆盖范围,提供120米的datasheet是validated户外运动在一个测试环境温度的26°c。
6、结果:拟议系统在病人身上的实际实施
在学校环境中的一间教室(带电脑)对三名健康受试者进行了为期三天的无线远程温度监测装置测试。他们在实验中坐着的时候,我们测量了他们的体温。传感器仅在测量过程中连接到车身上。当他们想放松的时候,就把传感器取下来,躺在可折叠的床上。
用户可以分配带有他/她的住院序列号标签的患者姓名。分配后,带有序列号的患者姓名将应用于数据库中的本地文件夹。图5(底部)显示了受试者的局部温度记录。温度记录保存在文本文件中,数据格式为“温度时间”。
在护士站,在线数据库实现中使用的两个主要组件是mysql数据库和php脚本。使用了名为sparkstation.net的在线托管服务器。每组患者信息包括协调员创建的温度、时间和日期。为了正确操作系统,用户接受了检索和提供正确患者信息的培训。使用不同颜色来指示高热患者有一个额外的特点;此外,如果标准偏差较大(或相当于陡坡),则会触发警报。在进行测试之前,作者已经获得了三名参与者的道德认证和知情同意。使用了图5(中心)中协调员集(护士站)的GUI。协调器组通过RS-232串行电缆连接到协调器计算机。每次协调器MCU接收到温度读数信息时,它都会将该信息发送到协调器的计算机。单击“更新图表”按钮后,GUI读取并生成特定患者和日期的温度记录图表。收到消息后,GUI将输入转换为实际温度读数。
确定了评价数据变化的统计信息,如均值和标准差。对于初步试验,每隔2分钟进行20分钟的记录和取样,以测试拟用系统。随后的温度记录每小时取样或采集一次。参与者平均体温为36.6(95%置信区间为35.9和37.3)。标准差为1.0(95%置信区间为0.7和1.8),中位数为36.9(95%置信区间为36.0和37.2)。
对3名年龄在28-30岁之间的健康男性受试者(P1、P2和P3)在3天内(名为d1、d2和d3)测试无线远程温度监测系统。每次测量之间的间隔设置为1小时,从上午1点开始。三名参与者的体温被记录下来并绘制在时间序列图上,如图6所示。p1、p2和p3在不同日期的统计平均温度分别为36.8°C、36.7°C和37.8°C,p1、p2和p3的统计标准差约为0.3°C。这些值是使用24小时内收集的温度数据计算得出的。
如图6所示,无线远程温度监测系统能够测量参与者从1到24小时的温度。最高标准偏差约为0.3°C,在整个试验期间,在封闭的建筑环境中处于0.3至0.5°C[16,17]的范围内。总之,该系统可以在0.3到0.5°C的分辨率范围内测量体温,并显示0.3°C的小标准偏差。
7、讨论
佩戴便携式温度监测装置的参与者的温度读数通过无线传输到监测他们的主站。体温测量数据存储在一个在线数据库中,允许用户在不与参与者在一起时访问数据库。
使用该设备的目标患者是普通病房的患者,而不是重症监护室(ICU),尽管每天监测一次足以检测到护士在普通病房周围看患者时出现的不良或其他问题,但该设备有助于为其他任务腾出时间,并降低风险。与接触传染病患者有关。在设备的帮助下,它提供了一个额外的预防措施,以确保正常病房的所有患者都能以最小的努力进行足够的温度监测。在对三名参与者在不同日期进行的测试中,我们观察到p1和p2的温度高于p3,特别是在第3天。这可能是因为2天后有些“疲劳”。我们确实怀疑温度传感器有问题,但当我们根据温度计校准温度时,情况很好。温度没有趋势的原因(如昼夜节律[18])是因为参与者实际上非常清醒(例如,他们在聊天和玩智能手机),而且他们没有真正进入睡眠状态。
8、结论
本文介绍了一种基于网络的MIWI无线腋窝温度远程监测装置。温度数据通过MIWI无线协议发送到连接到互联网的护士站。这种方法是由一个病人和协调器集设计,连接监测,传输,警报和记录温度的过程。对该装置进行的实验测试表明,该装置具有远程覆盖、0.3~0.5°C的温度分辨率和约0.3°C的小标准偏差。重要的是,该系统将有可能通过24小时连续监测患者的温度和降低工作压力来提高护理质量。普通病房的护理人员太多了。
远程温度监测装置将进一步发展成为一种具有即插即用功能的低成本产品,使未经培训的护士或医生能够在最少的帮助下使用。用户的软件界面将得到改进,并易于安装和下载。对于未来涉及远程监控的工作,将比较ZigBee和WiFi等不同无线网络协议的使用情况。医院最终将使用标准医用温度探头,如鼓室探头和标准一次性胶带。需要根据当前的测量技术对提议的系统进行进一步的评估。将研究隐私和安全保护以及向临床信息系统(CIS)的导出。
指导教师(签字):
年 月 日